Merrillville, IN
Munster, IN

Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
What Causes Toe Cramps?
Just like other parts of your body, your feet and toes have many muscles. These muscles can become cramped, leading to pain and difficulty walking. The pain is usually temporary and often goes away without treatment. Possible causes of toe cramps include having tight or weak muscles, a muscle injury, wearing poorly-fitted shoes, and being dehydrated. Sometimes, toe cramps can be a symptom of a more serious problem. For example, poor circulation can make the feet and toes ache and spasm, while nerve damage can cause pain, cramps, tingling, and numbness in the toes. Both of these conditions are often seen in patients who have diabetes. Another potential cause of toe cramps is arthritis, a condition that causes pain and inflammation in joints, including those in the toes. If you have persistent toe cramps that are bothering you, it is strongly suggested that you seek the care of a podiatrist.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
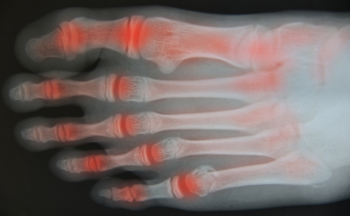
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Can Osteoarthritis Occur in the Ankles?
Osteoarthritis in the ankles is a very painful condition which causes the cartilage that protects bones in the ankle to deteriorate. This leads to bones rubbing against each other, swelling, stiffness, tenderness and intense pain in the ankle, and a decreased ability to walk or bend and flex your ankles. Several factors can increase your risk of developing osteoarthritis (OA) in the ankles, such as previous ankle injuries, recurrent high-impact stress on the ankles, misaligned joints, genetics, obesity and age. Your podiatrist can diagnose OA with a physical exam to test joint tenderness and swelling, X-rays, a gait analysis to assess your stride and foot and ankle biomechanics, and blood tests to distinguish OA from other forms of arthritis. There are many ways a podiatrist can help you manage the symptoms of OA, from lifestyle changes and physical therapy to various braces and orthotic devices, topical creams, pain relievers, and steroid injections. In severe cases of OA, surgery may be beneficial to remove spurs and loose cartilage, fuse the ankle to reduce pain, or replace damaged cartilage and bone with prosthetic parts (arthroplasty). If you believe you may have osteoarthritis in the ankle, it is suggested that you make an appointment as soon as possible to begin treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Why Some People Sweat Excessively on Their Feet
Thermoregulation is the body’s process of maintaining its core internal temperature, which is typically between 98°F and 100°F. Sweating is one of the mechanisms the body uses to cool down because as sweat evaporates it cools the skin, which lowers our internal temperature. Excessive sweating in specific areas of the skin is known as hyperhidrosis, or sometimes is referred to as plantar hyperhidrosis when it occurs in the feet. The specific cause of Hyperhidrosis is unknown, however its possible triggers are believed to include emotions, hormones, physical activity, or brain signals which inaccurately prompt sweat glands to overreact even when it is not necessary for thermoregulation. Sweat that sits stagnant on the skin of the feet can compromise the top layer of skin, making it more susceptible to bacteria which can create odor and even expose the body to more serious bacteria. Podiatrists have a variety of treatment options to help control this embarrassing and uncomfortable condition.
If you are suffering from hyperhidrosis contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to attend to all of your foot and ankle needs.
Hyperhidrosis of the Feet
Hyperhidrosis is a rare disorder that can cause people to have excessive sweating of their feet. This can usually occur all on its own without rigorous activity involved. People who suffer from hyperhidrosis may also experience sweaty palms.
Although it is said that sweating is a healthy process meant to cool down the body temperature and to maintain a proper internal temperature, hyperhidrosis may prove to be a huge hindrance on a person’s everyday life.
Plantar hyperhidrosis is considered to be the main form of hyperhidrosis. Secondary hyperhidrosis can refer to sweating that occurs in areas other than the feet or hands and armpits. Often this may be a sign of it being related to another medical condition such as menopause, hyperthyroidism and even Parkinson’s disease.
In order to alleviate this condition, it is important to see your doctor so that they may prescribe the necessary medications so that you can begin to live a normal life again. If this is left untreated, it is said that it will persist throughout an individual’s life.
A last resort approach would be surgery, but it is best to speak with your doctor to find out what may be the best treatment for you.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Hyperhidrosis of the Feet
Hyperhidrosis of the feet, also termed plantar hyperhidrosis, is characterized by excessive sweating of the feet that can be onset by any cause, such as exercise, fever, or anxiety. Most people suffering from hyperhidrosis of the feet also experience hyperhidrosis of the hands, or palmar hyperhidrosis. Approximately 1-2% of Americans suffer from this disorder.
Sweating is a healthy process utilized by the body in order to cool itself and maintain a proper internal temperature, which is controlled by the sympathetic nervous system. In individuals with hyperhidrosis, the sympathetic nervous system works in "overdrive", producing far more sweat than is actually needed.
Plantar hyperhidrosis is considered primary hyperhidrosis. Secondary hyperhidrosis refers to excessive sweating that occurs in an area other than the feet, hands, or armpits, and this indicates that is related to another medical condition, such as menopause, hyperthyroidism, or Parkinson's disease.
Symptoms of hyperhidrosis of the feet can include foot odor, athlete's foot, infections, and blisters. Because of the continual moisture, shoes and socks can rot which creates an additional foul odor and can ruin the material, requiring shoes and socks to be replaced frequently. In addition to the physical symptoms, emotional health is often affected as this disorder can be very embarrassing.
If left untreated, hyperhidrosis will usually persist throughout an individual's life. However, there are several treatment options available. A common first approach to treating hyperhidrosis of the feet is a topical ointment. Aluminum chloride, an ingredient found in antiperspirants, can be effective at treating hyperhidrosis if used in high concentration and applied to the foot daily. Some individuals can experience relief this way, while others encounter extreme irritation and are unable to use the product. Another procedure is the use of Botulinum Toxin A, commonly referred to as Botox. This is injected directly into the foot, and is effective at minimizing the sweat glands in the injected area. These injections must be repeated every 4 to 9 months.
If these treatments are ineffective, oral prescription medications may be taken in an effort to alleviate the symptoms. Again, some will experience relief while others do not. Going barefoot reportedly provides relief for most sufferers.
A final approach to combating hyperhidrosis of the feet is through surgery. Surgery has been less successful on patients with plantar hyperhidrosis than on those with palmar hyperhidrosis. It is only recommended when sweating is severe and other treatments have failed to work. This kind of surgery usually involves going into the central nervous system, and cutting nerves to stop the transmission of signals telling the foot to sweat.
What Can Custom Orthotics Do for My Foot Condition?
Custom orthotics are prescription devices that fit in shoes and are designed to distribute weight more evenly across the feet and minimize pressure on any given area. They can also correct an abnormal gait, reduce pain, and improve foot alignment. Since they are designed to address specific conditions and the individual foot structure of the patient, fit is critical. After a podiatrist examines the patient and diagnoses their underlying condition, they may determine that orthotics can be beneficial. They will then take an impression of the patient’s foot, usually with a 3D laser scan or plaster cast. Specific materials will be chosen to address the patient’s particular condition, and the orthotic will be created. The patient will come in for a fitting and any further customizations needed to ensure the device fits the patient’s shoes and is comfortable will be made. Orthotics can be prescribed for conditions such as arthritis, plantar fasciitis, heel spurs, bunions, hammertoes, flat feet, high arches and more. If you have any of these conditions, it is suggested that you make an appointment with a podiatrist to see if orthotics may be beneficial for you.
If you are having discomfort in your feet and would like to try orthotics, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.