Merrillville, IN
Munster, IN

Plantar Fasciitis Can Be a Painful Setback for Athletes
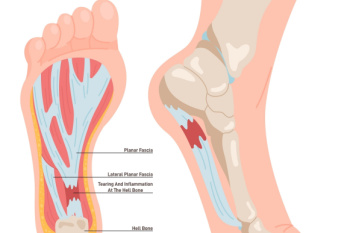
Plantar fasciitis is one of the most common causes of heel pain, and for athletes, it can be a game-changer. This condition occurs when the plantar fascia, the thick band of tissue running along the bottom of the foot, becomes inflamed from overuse, excessive impact, or improper biomechanics. Runners, basketball players, and dancers are especially prone due to repetitive foot stress. Sharp, stabbing pain is often worse in the morning or after long periods of activity. Ignoring it can lead to chronic discomfort and even compensatory injuries in the knees or hips. Treatment includes rest, stretching, wearing proper footwear, and sometimes custom orthotics to provide arch support. If you are an athlete eager to stay in the game, it is suggested that you seek care from a podiatrist.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Diabetic Neuropathy Foot Issues

Foot neuropathy is a common complication for those with high blood glucose levels, often linked to diabetes. High blood sugar can damage the nerves in your feet, leading to symptoms like tingling, numbness, burning sensations, or sharp pains. Some people may also experience weakness or loss of feeling, making it difficult to notice injuries or infections. Over time, this damage can worsen, potentially leading to balance problems or ulcers that may go unnoticed. A podiatrist can diagnose foot neuropathy through a physical examination and sensory testing. Treatment includes custom insoles to relieve pressure, medication to manage pain, or targeted exercises to improve mobility and strength. In some cases, they may recommend lifestyle changes to help control blood sugar levels. Proper foot care is critical to prevent further complications, as untreated neuropathy can lead to more severe issues. If you have foot neuropathy, it is suggested that you schedule an appointment with a podiatrist for expert care and guidance.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Explaining Charcot Foot

Charcot foot is a serious condition that affects the bones, joints, and soft tissues of the foot and ankle. It is most common in people with diabetes who have peripheral neuropathy. Charcot foot leads to inflammation that weakens the bones, making them more prone to fractures and dislocations. Because neuropathy reduces sensation, people may continue walking on an injured foot without realizing the extent of the damage. Over time, this can cause severe deformities, such as a collapsed arch, known as a rocker-bottom foot. Symptoms often include swelling, warmth, redness, and changes in foot shape. Without proper treatment, Charcot foot can increase the risk of wounds and infection, which may lead to limb loss. A podiatrist can assess the condition using imaging studies and clinical evaluations. Treatment typically involves immobilization with a cast or brace to prevent further damage. In more severe cases, surgery may be needed to restore foot stability and function. If you believe you have symptoms of Charcot foot, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Some foot conditions may require additional professional care. If you have any concerns, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
How Lupus Can Affect the Feet

Lupus is an autoimmune disease that can affect the feet, often causing pain, swelling, and circulation problems. Inflammation from lupus may lead to joint damage, resulting in conditions such as Jaccoud’s arthropathy, where the toes become misaligned, making walking difficult. Polyarthritis can also develop, causing persistent stiffness and discomfort in the foot and ankle joints. Many people with lupus experience Raynaud’s phenomenon, which reduces blood flow to the toes, leading to cold, numb, or discolored feet. This condition can make standing or walking painful, especially in colder temperatures. Lupus may also cause sores or blisters on the feet to heal slowly, increasing the risk of infection. Nerve damage linked to lupus can result in tingling, burning sensations, or loss of feeling in the feet. A podiatrist can help manage these symptoms by evaluating your foot structure, addressing circulation concerns, and recommending treatments that improve mobility and reduce pain. In severe cases, surgery may be needed to correct deformities. If you have foot pain that may be related to lupus, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment solutions.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
Causes of Ankle Pain

Ankle pain can arise from various conditions like sprains, arthritis, or tendonitis. A sprained ankle occurs when the ligaments are stretched or torn, causing swelling, bruising, and sharp pain, particularly when walking or standing. Arthritis can cause joint pain, stiffness, and swelling, often worse in the morning or after prolonged activity. Tendonitis happens when the tendons surrounding the ankle become inflamed, leading to pain, especially during movement or exercise. Depending on the cause, ankle pain can feel sharp, dull, or achy, and may limit your ability to walk or be active. Treatment options include rest, targeted exercises, anti-inflammatory medications, or custom orthotics. In more severe cases, a podiatrist may suggest injections or surgery to repair damaged tissues. This type of doctor can provide a precise diagnosis and create a treatment plan tailored to your needs, helping you regain mobility and reduce pain. If you are struggling with ankle pain, it is suggested that you schedule an appointment with a podiatrst for appropriate treatment solutios.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.














