Merrillville, IN
Munster, IN

Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Safe Removal of Corns on the Feet

When dealing with corns on the feet, it is important to prioritize safe removal techniques, particularly if you have underlying health conditions, like diabetes. Seeking professional help from a podiatrist is essential, especially if the corns are painful or if there are concerns about infection or other complications. A podiatrist may use various methods for safe corn removal, including trimming them with a small knife or applying salicylic acid patches to soften them. These procedures are performed in a controlled medical setting to minimize the risk of infection. Additionally, the podiatrist may address underlying structural issues that can contribute to corn formation, such as bunions or hammer toes. It is important to refrain from attempting corn removal yourself, especially for individuals with diabetes or circulation problems. If you have a problem with a corn on the foot, it is suggested that you schedule an appointment with a podiatrist for its safe removal.
If you have any concerns regarding your feet and ankles, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Reasons for Flat Feet

Flat feet, also known as pes planus, affect about 18 million adults in the United States, with an additional 8 million grappling with fallen arches. Flat feet often stem from the weakening of the posterior tibial tendon, which supports the arch of the foot. It can worsen after years of simple daily activity, like walking, running, and standing. While flat feet are normal in infants and toddlers, some individuals never develop arches, leading to persistent issues into adulthood. Distinguishing between flat feet and overpronation is important for an accurate diagnosis. With flat feet there is no visible arch whether seated or standing. Overpronation, however, is a biomechanical change in the way you walk that can contribute to fallen arches. In either case, seeking a professional evaluation from a podiatrist is essential if you suspect flat feet or experience pain related to flat feet. For a full exam and subsequent treatment plan, it is suggested that you schedule an appointment with a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Treatment Options for Plantar Fasciitis
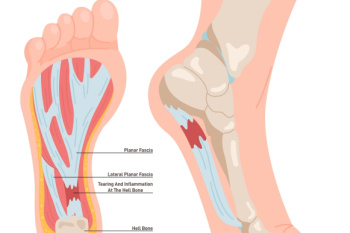
Plantar fasciitis, a common cause of heel pain, often necessitates employing a number of methods to alleviate symptoms effectively. Supportive therapies, such as targeted foot and calf stretches, can help to minimize pressure on the damaged plantar fascia, a band of tissue that runs from the toes to the heel under the foot. For more severe cases, corticosteroid injections may offer temporary relief from the pain. In addition, a shift toward performing low-impact exercises, like swimming or cycling, can help to maintain cardiovascular health while minimizing strain on the affected area. Customized orthotics, targeting the arch and swollen regions of the foot, have been shown to provide relief as well as prevent future occurrences of plantar fasciitis. Healing from plantar fasciitis typically occurs within 12 to 18 months with nonsurgical methods. For individualized care from the pain and inconvenience of plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Ways Smoking Affects the Feet

Smoking can significantly affect foot health by restricting blood flow and impairing bone growth and healing processes. Nicotine in tobacco narrows blood vessels, reducing circulation to the extremities. Further, chemicals in cigarettes weaken vessel linings, which promotes plaque buildup and further compromises blood flow to the feet. This increases the risk of conditions like peripheral arterial disease and blood clot formation. A diagnosis typically involves blood tests, comparative blood pressure exams, and imaging studies. Treatment strategies vary, often incorporating lifestyle adjustments, such as exercise and a balanced diet, along with managing cholesterol and blood pressure levels. Additional risk factors that affect foot health include diabetes, high cholesterol, and high blood pressure. While quitting smoking is vital, consulting with a podiatrist is an essential part of the comprehensive care needed. A podiatrist can offer guidance to mitigate smoking-related foot problems. If you're a smoker and notice that you are having problems with your feet, it is suggested that you add a podiatrist to your team of healthcare experts.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.