Merrillville, IN
Munster, IN
October 2023
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
The Importance of Podiatric Care Among Diabetics

Consulting a podiatrist for diabetic foot care is essential for individuals with diabetes. Diabetes can cause neuropathy, which is a loss of sensation in the feet, making it difficult for patients to feel injuries, blisters, or sores. This numbness can lead to unnoticed and untreated wounds, which can quickly become infected due to compromised immune responses often seen in diabetic patients. In addition to neuropathy, diabetes can cause poor circulation, making it harder for wounds to heal and increasing the risk of infections. If untreated, these infections can lead to ulcers and gangrene. If you have diabetes, it is strongly suggested that you make regular appointments with a podiatrist to maintain overall foot health and reduce the risk of foot complications.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Causes of Foot Stress Fractures

Foot stress fractures, though they can happen to anyone, often have identifiable causes and risk factors. One of the leading causes of stress fractures is a sudden increase in activity. This increase can encompass frequency, duration, or intensity. It is particularly common among athletes pushing their boundaries, like marathon runners who ramp up their mileage too quickly. Changing the surface upon which you exercise is another factor to consider. Transitioning from a soft, forgiving surface like an indoor track or turf to a harsh, unforgiving one like a concrete sidewalk can place undue stress on the bones of your feet. Improper technique is a hidden enemy, as it can stem from other foot conditions, like blisters or bunions. When people adjust their gait to avoid pain or discomfort, they may inadvertently place extra stress on certain bones in the foot. Footwear matters more than you might think. Ill-fitting, flimsy, stiff, or worn-out shoes can contribute significantly to the development of stress fractures. It's not just athletes who need to be aware because even non-athletes can experience these injuries after walking extensively on uneven terrain, common during vacations. For more information on dealing with foot stress fractures, it is suggested that you make an appointment with a podiatrist.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Ahmad Elsamad, DPM from The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Symptoms of Morton's Neuroma
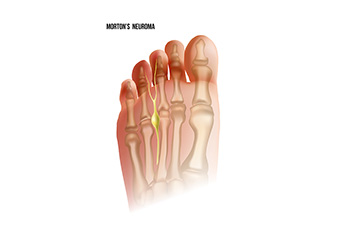
Morton's neuroma is a nerve condition in the feet, often causing discomfort and pain. The primary symptom is a sharp or burning pain typically felt between the third and fourth toes, but it can also extend to the ball of the foot. Individuals with Morton's neuroma may describe a sensation of having a pebble or lump inside their shoe. Additionally, many people experience numbness, tingling, or a feeling akin to standing on a fold in their sock. Pain tends to worsen with walking, wearing tight shoes, or putting pressure on the affected area. People may feel relief by removing their shoes or massaging their foot. These symptoms can be intermittent or chronic, affecting daily activities and quality of life. Recognizing these signs is essential for early intervention and appropriate management of Morton's neuroma. If you suspect you may have this condition, it is suggested that you seek medical advice from a podiatrist who can provide you with an accurate diagnosis and tailored treatment plan.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Congenital Foot Problems
A congenital foot problem is a problem affecting the feet, toes, and/or ankle that a child is born with. Several issues with a child’s feet can occur congenitally. Such problems include clubfoot, vertical talus, tarsal coalition, polydactyly, macrodactyly, and cleft foot. Some of these problems have a genetic basis, with someone in their family history having a gene causing the condition, and some are simply an anomaly.
The following are specifics about a few of these conditions:
- Clubfoot, also called congenital talipes equinovarus or talipes equinovarus, is When the tendons of the foot shorten, the bones are of an unusual shape, and the Achilles tendon is tight, causing an inward and downward pointing of the foot. The soles of the feet might also face each other. In most cases of clubfoot, both feet are affected. If not treated, the affected child will walk on the sides of their feet or ankles.
- Polydactyly is a condition where the child has more than five fingers or toes on either or both feet. Presentation usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus is where the talus bone forms in the wrong position, other bones in the foot do not line up properly, the front of the foot points up, and the bottom of the foot is stiff, has no arch, and usually curves out. This can occur in one or both feet and if left untreated, can lead to serious disability or discomfort as the child grows.
- Tarsal coalition is when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot. The tarsal bones, located toward the back of the foot and in the heel, are the ones affected. This condition is often present at birth, but signs of the disorder usually come on in early adolescence.
- Cleft foot is a rare condition where the foot has missing toes, a V-shaped cleft, and other anatomical differences. Surgery can often help improve the foot’s function since the heel remains normal and is what is most needed for walking. The main issues with this affliction are whether the affected foot can fit into a shoe and the shape and appearance of the foot.
- Macrodactyly is when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue. Having this condition makes it harder for the child to use the affected foot for certain activities.
Congenital Foot Anomalies

Toe defects can be present at birth, known as congenital anomalies. These can range from incomplete formation to extra toes. One cause could be amniotic band syndrome, where strands from the amniotic sac entangle around the fetus, restricting growth. Polydactyly refers to toes, which can be fully functional or just a flesh nub. Syndactyly involves webbing or fusion of toes. In simple cases, only soft tissues are fused, but in complex cases, bones are also fused. These defects can also be part of genetic syndromes such as Apert syndrome. Diagnosis often involves ultrasounds before birth and X-rays after birth. Genetic testing may also be done, particularly if other family members have similar issues or a genetic syndrome is suspected. Treatment usually involves surgery to correct the defect or remove extra digits. Prosthetics may be used for missing toes. If your child has been born with extra toes, it is suggested that you make an appointment with a podiatrist as quickly as possible for the best treatment for your child that will help ensure growing up with little to no impact on their mobility.
Congenital foot problems require immediate attention to avoid future complications. If you have any concerns, contact Ahmad Elsamad, DPM of The Institute of Foot & Ankle Reconstructive Surgery . Our doctor can provide the care you need to keep you pain-free and on your feet.
Congenital foot problems are deformities affecting the feet, toes, and/or ankles that children are born with. Some of these conditions have a genetic cause while others just happen. Some specific foot ailments that children may be born with include clubfeet, polydactyly/macrodactyly, and cleft foot. There are several other foot anomalies that can occur congenitally. What all of these conditions have in common is that a child may experience difficulty walking or performing everyday activities, as well as trouble finding footwear that fits their foot deformity. Some of these conditions are more serious than others. Consulting with a podiatrist as early as possible will help in properly diagnosing a child’s foot condition while getting the necessary treatment underway.
What are Causes of Congenital Foot Problem?
A congenital foot problem is one that happens to a child at birth. These conditions can be caused by a genetic predisposition, developmental or positional abnormalities during gestation, or with no known cause.
What are Symptoms of Congenital Foot Problems?
Symptoms vary by the congenital condition. Symptoms may consist of the following:
- Clubfoot, where tendons are shortened, bones are shaped differently, and the Achilles tendon is tight, causing the foot to point in and down. It is also possible for the soles of the feet to face each other.
- Polydactyly, which usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus, where the talus bone forms in the wrong position causing other bones in the foot to line up improperly, the front of the foot to point up, and the bottom of the foot to stiffen, with no arch, and to curve out.
- Tarsal coalition, when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot.
- Cleft foot, where there are missing toes, a V-shaped cleft, and other anatomical differences.
- Macrodactyly, when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue.
Treatment and Prevention
While there is nothing one can do to prevent congenital foot problems, raising awareness and receiving neonatal screenings are important. Early detection by taking your child to a podiatrist leads to the best outcome possible.
If you have any questions please feel free to contact our offices located in Merrillville, and Munster, IN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Gout Pain Can Be Managed
Taking Care of Elderly Feet
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.